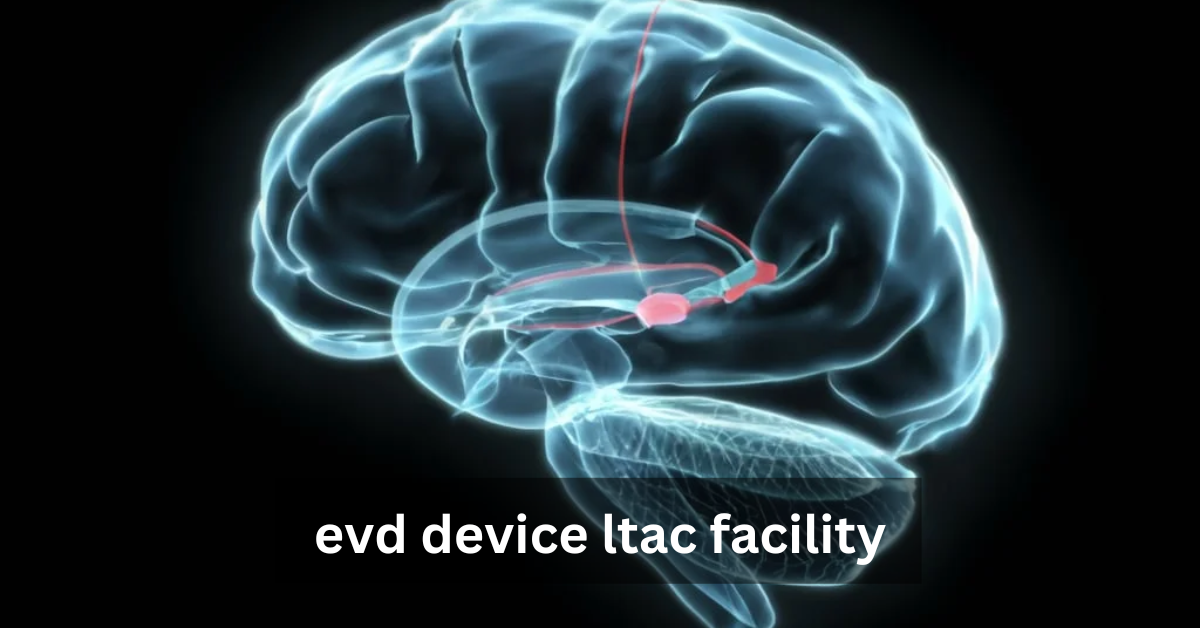
An External Ventricular Drain (EVD) is a device used to drain cerebrospinal fluid (CSF) from the brain, often used to manage intracranial pressure (ICP) in patients with neurological conditions like hydrocephalus or traumatic brain injury.
Learn about the key protocols in infection control, monitoring intracranial pressure, and providing rehabilitation.
An External Ventricular Drain (EVD) is a medical device designed to manage intracranial pressure (ICP) by draining excess cerebrospinal fluid (CSF) from the brain. It is an essential tool for patients suffering from neurological conditions like hydrocephalus, traumatic brain injuries (TBI), or subarachnoid hemorrhages. By regulating the flow of CSF, the EVD helps alleviate pressure on the brain, which could otherwise lead to devastating consequences, such as brain herniation or stroke.
Understanding Long-Term Acute Care (LTAC) Facilities
Long-Term Acute Care (LTAC) facilities specialize in providing intensive, extended care for patients with severe, often chronic medical conditions. These facilities cater to individuals who require more than just standard care but are not yet in need of full intensive care unit (ICU) support. For patients using an EVD, LTAC facilities offer the crucial combination of medical expertise, constant monitoring, and long-term rehabilitation support needed to manage complex neurological conditions.
Importance of Combining EVD Devices with LTAC Care
When patients with neurological issues, such as traumatic brain injury or hydrocephalus, require an EVD, LTAC facilities become critical in managing their recovery. The combination of EVD management and LTAC care ensures that patients receive 24/7 monitoring, infection control protocols, and expert neurological interventions. This integrated approach helps in preventing complications, managing ICP, and guiding patients through the often long and challenging rehabilitation process.
How EVD Devices Work: A Closer Look
Cerebrospinal fluid (CSF) is a clear liquid that surrounds the brain and spinal cord, providing protection and removing waste products. The regulation of CSF is vital for maintaining normal intracranial pressure (ICP). When excess CSF accumulates due to conditions like hydrocephalus or a traumatic brain injury, it can cause dangerous spikes in ICP, leading to severe neurological damage. An EVD device helps manage this process by continuously draining the excess fluid and maintaining balanced pressure levels.
The Mechanics of an External Ventricular Drain
The EVD device consists of a catheter inserted into the brain’s ventricles, connected to an external collection system. This system allows healthcare professionals to continuously monitor CSF levels and adjust drainage as necessary. The device is typically used in the short term but may remain in place for weeks or even months, depending on the patient’s condition and recovery progress. Its design ensures that fluid is removed from the brain while minimizing the risk of infection and ensuring the system’s integrity.
When and Why EVD Devices are Needed in Neurological Care
EVD devices are primarily used in conditions where there is an urgent need to manage increased intracranial pressure. These include cases of hydrocephalus, subarachnoid hemorrhage, traumatic brain injury, and intraventricular hemorrhage. The decision to use an EVD is typically made when less invasive methods are insufficient, or there is a risk of significant brain damage due to the buildup of cerebrospinal fluid.
The Role of Levd device ltac facility in Managing EVD Devices
evd device ltac facility are equipped with advanced medical technology and a specialized team of healthcare professionals who are trained to manage critical and complex conditions. These settings provide patients with the round-the-clock attention they require, particularly for individuals with neurological conditions requiring continuous monitoring. The environment is tailored for extended care, offering services ranging from ventilation support to physical rehabilitation. This makes LTAC facilities uniquely suited for managing patients with EVD devices who need ongoing ICP monitoring and support.
Managing an EVD device is not a routine task and requires specialized training. The device must be carefully maintained to avoid complications such as infection, improper drainage, or changes in CSF levels that could affect brain function. LTAC facilities are equipped with professionals who are experienced in dealing with these complexities, ensuring that any fluctuations in ICP are immediately addressed and that patients remain stable during their recovery process.
LTAC facilities offer significant benefits for patients with ICP issues. Continuous monitoring and early intervention in the case of complications are vital to preventing long-term damage. In LTAC settings, patients are closely observed for signs of increased ICP or infections, allowing medical staff to act quickly. Additionally, LTAC staff are trained to adjust the EVD system as needed to ensure that pressure levels remain within safe ranges, promoting optimal brain health.
Patient Care in an EVD Device LTAC Facility
In LTAC facilities, patient care involves a multidisciplinary approach. Neurologists, neurosurgeons, critical care nurses, and rehabilitation therapists collaborate to manage the patient’s condition. For patients with an EVD, this team is essential in coordinating care, adjusting the device, and monitoring neurological progress. The combined expertise of these professionals ensures that each patient receives the most comprehensive care possible.
Nurses play a pivotal role in daily monitoring of the EVD system, ensuring that drainage is functioning properly and looking out for signs of infection. Neurologists and neurosurgeons are involved in assessing the patient’s neurological status and making any necessary adjustments to the EVD settings. Surgeons may be required for follow-up procedures or to adjust the device if complications arise. This constant collaboration among healthcare professionals ensures the highest quality of care.
The monitoring and adjustment of EVD devices is a delicate task. Nurses and medical staff track the amount of fluid drained, assess changes in ICP, and adjust the drainage settings to match the patient’s needs. This careful process helps prevent complications like brain herniation or fluid imbalances. Furthermore, continuous monitoring ensures that any changes in the patient’s condition are addressed immediately, reducing the risk of irreversible damage.
Infection Control and Prevention in EVD Device Management
One of the most significant risks associated with EVD devices is the potential for infection. The system provides direct access to the brain, which makes it vulnerable to bacterial infections like meningitis or ventriculitis. These infections can severely complicate recovery, requiring immediate medical intervention. As such, infection prevention is a primary concern in LTAC facilities.
LTAC facilities are equipped with stringent infection control protocols to mitigate the risk of complications. Sterile techniques are followed when handling the EVD system, and healthcare professionals are trained to monitor for early signs of infection. Regular cleaning of the insertion site, changing of the drainage system, and close monitoring of the patient’s condition help to reduce the chances of infection. Preventing infections is a top priority to ensure the best recovery outcomes for the patient.
Infections like meningitis and ventriculitis can develop if the EVD system is not properly managed. These conditions can cause significant neurological damage, leading to long-term complications or even death. To prevent such outcomes, LTAC facilities have infection control specialists who ensure that every aspect of the EVD device management is sterile. Monitoring for early signs of infection, such as fever or changes in the appearance of CSF, allows healthcare teams to act swiftly and effectively.
Managing Intracranial Pressure in LTAC Facilities
The primary role of the EVD device is to control ICP by draining excess cerebrospinal fluid. By maintaining a balanced pressure level, the device helps prevent the brain from being damaged by excess fluid buildup. Managing ICP is critical for the survival and recovery of patients with severe brain injuries, hydrocephalus, or other neurological conditions.
Continuous ICP monitoring is a cornerstone of care in LTAC facilities. Real-time data from the EVD system allows healthcare providers to track changes in pressure and adjust the drainage settings accordingly. This proactive approach ensures that ICP remains within safe levels, significantly improving the chances of a positive recovery.
Proper ICP management is directly linked to patient recovery. When ICP is controlled, the brain is able to heal, and neurological function is preserved. By combining EVD management with comprehensive LTAC care, patients are more likely to experience favorable outcomes, including a reduction in brain damage and improved recovery times.
Rehabilitation and Recovery with EVD Devices in LTAC
Neuro-rehabilitation plays a crucial role in recovery for patients who have experienced brain injuries or neurological trauma. LTAC facilities provide specialized rehabilitation services, such as physical therapy, occupational therapy, and speech therapy, to help patients regain function and independence. These therapies are particularly important for patients recovering from traumatic brain injuries or those with long-term neurological conditions.
Once a patient’s condition stabilizes in the acute phase, LTAC facilities begin the process of transitioning to long-term recovery. This includes gradually reducing dependence on the EVD device as the patient’s brain function improves. Rehabilitation programs focus on strengthening
Challenges and Considerations in EVD Device LTAC Management
Despite the critical role EVD devices play in managing intracranial pressure (ICP), they are not without complications. Some of the most common issues include mechanical problems, such as blockages or dislodgement of the catheter, and more severe complications like infections, including ventriculitis and meningitis. These complications can delay recovery, lead to long-term neurological damage, or even pose life-threatening risks if not managed promptly. It is crucial that LTAC facilities have rigorous protocols in place to detect and address such complications as quickly as possible.
LTAC facilities often face staffing challenges, particularly in highly specialized areas like neurocritical care. The specialized nature of EVD device management requires highly trained healthcare professionals who can monitor and adjust devices in real-time. Unfortunately, a shortage of trained nurses or neurologists in some regions can create difficulties in ensuring that every patient receives the level of care they need. To address these challenges, LTAC facilities are increasingly turning to technology, such as telemedicine and remote monitoring, to ensure continuous care even during staffing shortages.
Technological Advancements in EVD Device LTAC Care
Advanced ICP monitoring systems now allow healthcare teams to remotely track patients’ brain pressure in real-time, reducing the need for constant manual checks. In addition, automated alarm systems can alert healthcare providers to sudden changes in ICP or fluid drainage, allowing for faster intervention when needed. These technological advancements not only improve patient outcomes but also streamline care, allowing LTAC staff to focus on other aspects of patient recovery.
The future of EVD device management in LTAC facilities looks promising, with ongoing innovations aimed at improving patient safety and recovery times. Future devices may incorporate more advanced sensors that provide more accurate, real-time data about the patient’s condition, reducing the need for invasive procedures. Additionally, developments in remote monitoring and telemedicine could make it easier for specialists in different locations to assist in the care of EVD patients, further enhancing the quality and accessibility of care.
Telemedicine has already made its way into LTAC facilities, enabling remote consultations with neurologists, neurosurgeons, and other specialists. This technology is particularly useful for managing EVD devices, as specialists can monitor data from afar and adjust treatment plans without needing to be physically present. Telemedicine also allows for quicker responses to potential complications, minimizing the risks associated with delays in treatment.
Conclusion
evd device ltac facility offer a unique and essential environment for the management of EVD devices, providing around-the-clock care, specialized medical expertise, and state-of-the-art technology to ensure optimal patient outcomes. The combination of medical professionals, advanced monitoring, and infection control protocols makes LTAC care indispensable for patients with serious neurological conditions that require the use of an EVD.
LTAC facilities significantly enhance patient outcomes by providing a comprehensive, multidisciplinary approach to care. From preventing infections and managing ICP to facilitating rehabilitation and recovery, these facilities offer the level of care needed to give patients the best chance of a full recovery. By ensuring that EVD devices are carefully managed and that patients are constantly monitored, LTAC facilities help patients recover and regain function after severe neurological events.
The future of EVD management in LTAC settings is bright, with continuous improvements in technology and care protocols. As more advancements in monitoring devices and telemedicine are implemented, LTAC facilities will become even more efficient and effective in managing these complex medical conditions. This will ultimately lead to better care, faster recovery times, and enhanced quality of life for patients who depend on EVD devices to manage their neurological health.
Frequently Asked Questions
Why is LTAC care important for patients with an EVD device?
LTAC facilities provide specialized, long-term care for patients who need continuous monitoring and support, particularly when managing complex conditions like intracranial pressure or EVD devices. This level of care ensures optimal recovery and reduces the risk of complications.
What are the risks associated with EVD devices?
Infection, such as meningitis or ventriculitis, is a significant risk when using an EVD. There are also risks related to improper drainage, blockages, and catheter displacement, which can lead to increased intracranial pressure.
How does technology assist in EVD management in LTAC facilities?
Technology such as real-time ICP monitoring and automated alarms allows healthcare providers to track patient data and make immediate adjustments to the EVD device, ensuring optimal management of the patient’s condition.
What role does rehabilitation play in the recovery of EVD patients?
Rehabilitation, including physical therapy and occupational therapy, plays a crucial role in helping EVD patients regain function and independence. LTAC facilities offer neuro-rehabilitation programs tailored to support recovery after brain injury or surgery.
Stay in touch to get more updates & alerts on Picnob! Thank you